from Leadership Medica n. 10/2006
Abstract
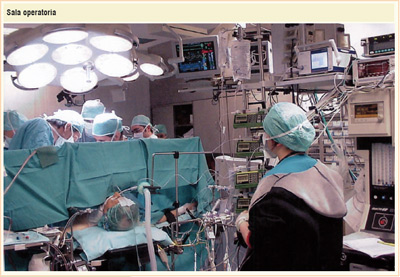
The first general anesthesia with ether was performed by dr. Thomas Morton the Ether day, October 16th 1846, on a patient at the Massachusetts General Hospital in Boston. The present paper, after a short history of the beginning of the fight against pain, reports on the last 160 years from the ether day and describes the discoveries, the innovations and the continuous and relentless pharmacological, physio-pathological and clinical progresses that characterized the development of modern anesthesiology after the end of World War II. We will describe the pillars of general anesthesiology, loco-regional anesthesiology, local anesthesiology and we will show the therapeutic choices according to the different surgical procedures. We will briefly discuss on the devices routinely utilized in the operating rooms for the monitoring of life functions trying to make the reader figure out what happens in the operating theater. In brief, we will try to explain what is anesthesiology.
We will finally analyze the role of a new profession, the anesthesiologist/intensive care doctor, that was created "only" fifty years ago. This new branch of medicine with the time run acquired further skills like the resuscitation, the pain therapy, the hyperbaric therapy and more recently the field of organ donation and transplantation with important ethical and deontological implications.
Summary:
- Introduction
- General anesthesiology
- Local and loco-regional anesthesia
- We will now elucidate the role of the anesthesiologist
Introduction
We prepared this article for the prestigious journal Leadership Medica with a little proud and a great sense of responsibility since it gives us the opportunity to describe what is anesthesiology and who is the anesthesiologist, a specific clinical branch and a new profession both derived from the necessity to fight pain.It seems appropriate to start with a brief (but long in time length) history of the fight against pain that comes from the old times of our ancestors since "pain is contemporary to the appearance of homo sapiens". Empirical methods, strange remedies and systems, bloody techniques characterized in the old history the solitary war of the man against pain. Hippocrates (3rd century B.C.) was told to introduce a less empiric method to induce a state of unconsciousness with a sponge soaked with mandragora and opium (the "sleepy sponge" later used as the symbol of the Scientific Society of Italian Anesthesiologist).
The term "anesthesia" was introduced in the 50 A.C. by a Greek doctor, Dioscorides, who studied the sleep and the insensitivity induced by mandragora. The latter seemed to be the most efficient method to perform "an attempt of anesthesia" until the XVI century when mandragora was associated with the opium or with the cocaine contained in the leaves chewed by the Indios. In the meantime the surgical operations were performed "in corpore vili" with great velocity and skill to shorten the pain length or using the carotid compression to induce a lost of consciousness (an often deadly technique), or with restraint devices or with ice (the surgeon Parè used it for an amputation in 1564) or with different concoctions applied on wounds or swallowed ("panaceas"). Between the XVIII and the XIX century important advancements were achieved in the field of the human sciences and in particular chemistry, biology, anatomy, physiology and pharmacology.
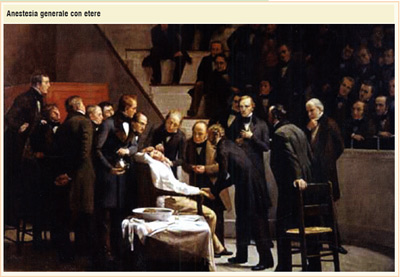
At the beginning of the XVIII century Davy discovered the nitrogen protoxide (N2O-"laughing gas") and his disciple Faraday found the sulphuric ether in 1818, and in 1831 chloroform was purified. Although such "drugs" are not used for humans these scientists can be considered the promoters of modern anesthesiology. Following a frustrating attempt of a tooth removal with nitrogen protoxide by Horace Wells, one of his disciples, W. T. Morton, the 16th of October 1846, in front of many doctors in the main hall of the Massachusetts General Hospital in Boston, removed a big neck tumor from a "sleeping" patient that inhaled ether vapors. This was the ether day, the beginning of modern anesthesiology. The man is not alone anymore in the fight against pain. The use of ether became quickly very popular in many countries and initiated a further era of discoveries and inventions: the syringe(1851), the chloroform, the curare, the barbiturates, the morphine derivates, the tracheal intubation, the cocaine (for topic use). Two techniques still used nowadays, peridural and subarachnoid anesthesia, were introduced at the end of the XIX century. All these advancements continued in the XX century and were collected in 1914 in a specific scientific journal named "Journal of Anaesthesia and Analgesia": this represented the first acknowledgement to this new branch of medicine. Many scientists (specially foreigners) achieved scientific observations and clinical applications in the field of general anesthesia and loco-regional anesthesia in the time between the world wars with a significant advancement of the discipline. Among the many foreign authors are worth to be remembered also two Italians: Dogliotti (surgeon who in 1931 trialed the use of alcohol in the peridural space) and Bovet (Nobel prize who in 1947 discovered and prepared a kind of curare, the gallamin). From 1950 to now anesthesiology made great efforts from the discovery of new inhalation anesthetic drugs, new molecules for pain control, new myo-relaxants, new anesthetic techniques, more sophisticated apparels for ventilation and monitoring and mostly from new acknowledgments of the physiology and the physiopathology of the intra- and post-surgical phases. In Italy the modern anesthesiology breaks in and spreads after World War II through the work and the intuition of few true pioneers who migrated abroad (specially in U.K.) and came back with great experience, thus starting the creation of the present "army" of Italian anesthesiologists.
General anesthesiology
This short history might explain what is anesthesiology. Nevertheless to better answer to the first question ("what is anesthesiology?") seems appropriate also to fully elucidate how anesthesiology is performed. As previously described the term anesthesia was introduced by the Greek doctor Dioscorides, literally meaning "absence of sensitivity". The term was later added with other meanings such as "anesthetic sleep" (narcosis). The latter is a drug-induced, "para-physiologic" sleep (different form the physiologic sleep and the pathologic sleep or coma), that is provoked by drugs (anesthetics) either injected intra-venous or inhaled. These drugs are able to induce the sleep in few minutes targeting the ascending reticular matter of the brain that is "depressed", thus stopping the connection with the superior centers and the cortex, the part of the brain appointed to consciousness, watch, affection and interpersonal relations. Administration of these drugs by injection (pentotal, propofol) and by inhalation (nitrogen protoxide, halotane, sevoflurane, desflurane) makes the patient sleep deeply. However this is not enough for a surgical operation and it is necessary to raise the pain threshold with the administration of morphine-derived analgesics, able to avoid completely all the pain stimuli produced by the scalpel. Finally, to facilitate the surgical procedure muscle paresis is induced by administration of curare. In this setting the tracheal intubation and the connection to the automatic breather becomes necessary due to the absence of spontaneous breathing.

During this first phase of induction, using the anesthetics, the analgesics and the curare, the patient sleeps deeply, is protected from any pain stimulus, is "curarized" (paralyzed) and breaths artificially. The surgical operation is ready to start. The second phase of anesthesia, the maintenance, may last for many hours during the surgical operation with the intra-venous administration of further doses of analgesics, curare and anesthetics (the latter can be replaced with anesthetics by inhalation) in order to maintain even levels of sleep, analgesia and curarization, being the patient ventilated by the breather. An even level of narcosis avoids (and must be avoided) the risk to lighten the sleep during the intervention (the so-called "awareness" phenomenon).
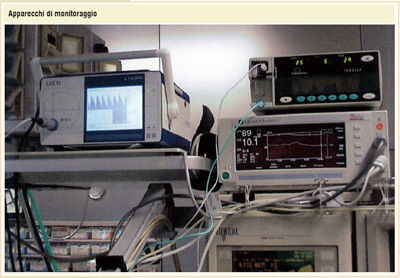
The third phase of anesthesia is the awakening. At the end of surgery the narcosis is progressively decreased (stopping the administration of anesthetics) and the curare is stopped (with resumption of spontaneous breathing). The patient is estubated and detachment from the breather: now the operated patient is awake and conscious, breaths autonomously and is free from pain. He/she can return to his bed provided of control of the post-surgical pain. The latter has been the focus of the national campaign of the Ministry of Health called "Hospital without pain" in 2001. General anesthesia with these modern, highly tested and easy-to-handle drugs can be considered a safe clinical procedure since it is performed thousands times a day in the operating rooms all around the world. The safety of the procedure is warranted by the presence of the anesthesiologist at the operating room bed. This allows the continuous monitoring of all the life functions by means of sophisticate (and expensive) apparels able to assist the surgical procedure to the end and to correct possible modifications/alterations of the circulatory, respiratory, renal and metabolic functions and more.
Local and loco-regional anesthesia
Besides general anesthesia local (or superficial) anesthesia, percolation anesthesia (blocking nerve terminations with local anesthetics like lidocain, mepivacain, bupivacain, ropivacain), troncular anesthesia (administering the local anesthetics close to main nerve trunks for operations on upper and lower limbs) and loco-regional anesthesia can be encountered. The latter technique has been progressively and largely utilized in the recent years. It consists in the injection of the local anesthetic (sometimes plus an opioid) in the epidural space (the so-called "peridural anesthesia") or in the subdural space (the so-called "spinal anesthesia"). The consciousness of the patient is preserved and only the area undergoing is made "insensitive". This technique is excellent for orthopedic surgery (lower limbs), urologic surgery (prostate), gynecological surgery and other surgery (varixes, hemorroids). The combination of general and loco-regional anesthesia (combined anesthesia) can be used in some kinds of surgery. In conclusion, anesthesiology allows to use a very wide spectrum of techniques that help the surgeon and support the sentence "the great efforts made in the last 30 years by the modern surgery are (also) due to the modern anesthesiology". Thus, anesthesiology allows to perform more and more complex operations (cardiac surgery, neurosurgery, thoracic surgery, pediatric surgery, organ transplantation) on a wide spectrum of patients (from immature newborns to elders) in the presence of associated diseases that may complicate the surgical operation.
We will now elucidate the role of the anesthesiologist
During and right after the World War II the anesthesia with ether was administered to the patients in the operating room by nouns and some rudimental technique of narcosis were performed by the surgeon themselves. At the and of the 50' the settlement of the first hospital departments of anesthesiology (by Borsellino, 1954) finally discredited the old and bad aphorism "the anesthesiologist is nephew of the noun and son of the surgeon". The first residency programs in anesthesiology were established and now reached the number of 39 (uniformed to the European standards, four year courses). Within these programs all the anesthesiologists studied and trained themselves in the operating rooms in the last 50 years.
There are currently more than 10.000 anesthesiologists in Italy. They are all skilled and serious professionals, especially the young ones who are trained day by day by the scientific society of anesthesiology (SIAARTI whose motto is "divinum opus sedare dolorem").
The anesthesiologist is therefore a specialist, scientifically and clinically trained in the residency programs who works in and outside the operating rooms before and after the operation, performing the so-called peri-operatory medicine. The latter represented the goal of the anesthesiologists for years: i.e. to completely assist the patient undergoing the operation through the application of anesthesia; to control the life functions or to resume them through the monitoring; to effectively collaborate with the surgeon (with the precious and often neglected assistance of the nurses); to avoid the risks of human mistakes that are possible in a stressful job where the maximum attention, skill and concentration are always required.
It should not be underestimated that serious or deadly complications might happen in the operating room. These events are often emphasized by the media as examples of "bad healthcare". Nevertheless the average of deadly complications is about 1 every 100.000 anesthesias. In these cases a variety of pathogenetic factors can be encountered whose occurrence must be discussed in the judge since the law demands the professional activity to be diligent, skilled and prudent.
The professional attitude of the anesthesiologist to the support of life functions makes him the specialist of resuscitation. The intensive care units, also called "multi-purpose intensive care units" are special departments established in Italy at the end of the 60' (by Mariotti in 1968), where acute or chronic patients are admitted with one or more life-threatening deficient life functions. Several different diseases can be responsible of this situation like multiple traumas, acute cardio-respiratory failure, shock, intoxication (exogenous or endogenous), severe metabolic impairment, post-surgery of critical patients and many others.
The intensive care doctor has a great experience acquired in the operating room during the training and thus takes care and handles the critical patients. He/she is supported by specifically trained nurses and by special apparels and specific devices. In these departments (every hospital is provided with an intensive care unit) a sort of "cutting edge medicine" is performed every day for 24 hours aimed to save human lives and to avoid unnecessary over-treatments or under-treatments, banishing euthanasia. These topics are frequently debated and need a specific legislation at least for what is regarding the "biologic will" (or"living will").
These arguments all need a separate discussion. As regards legal matter, the intensive care doctor has fully accepted the meaning of the 1994 law on brain death ascertainment.
In case of brain death, ascertained by the complete absence of all brain functions (as by the above mentioned law that is one of the strictest in Europe), the intensive care doctor facilitate the process of organ donation and transplantation, once assumed that there is no specific opposition. This is a new chapter of modern medicine. Transplantation of livers, hearts, lungs (life-saving organs for patients in waiting list) and also kidneys, corneas, bones and skin represents a new frontier of surgery. It also holds a great ethical and social value that can be outlined in the sentence "to donate life to others from the death of a single" that is totally assumed by the intensive care doctor. The intensive care doctor may also act outside the intensive care as physician of the 118 national emergency care service providing safe interventions to critical patients on the site where the emergency took place.
The skill acquired in the operating room with the administration of analgesics and nerve blockers allowed to develop the antalgic therapy.
Control of chronic pain (tumor-derived or not) is often on behalf of the anesthesiologist due to his specific knowledge of physio-pathology. In our country specialized "Pain Clinic" and "Hospices" grew-up where the anesthesiologists together with the oncologists treat patients with end-stage neoplastic diseases.
Anesthesiologist are also responsible for the handling of the hyperbaric chambers where are treated all the patients suffering from acute conditions like gas embolism (diver disease) and gas gangrene which benefit from hyperbaric oxygen-therapy. Anesthesiology is not only by far an effective support to surgery.
Once outside the operating room the anesthesiologist works in other clinical settings as intensive care, antalgic and hyperbaric therapy and extra-hospital emergency care. In these settings the anesthesiologist carries on his "vocation" towards the suffering patient looking at other medical branches and thus achieving the multidisciplinary approach that is the milestone of modern medicine.
Professor Gerardo Martinelli
Reparto di Anestesia e RianimazionePoliclinico S. Orsola Malpighi - Bologna



